Introduction
Welcome to JointPro Physical Therapy's resource about Osteoporosis.
Osteoporosis is a common bone disease that develops when the body loses too much bone mass, does not regenerate enough new bone tissue, or both issues occur. Bones mainly consist of calcium and phosphorus, but the level of these essential minerals dramatically decreases in patients with osteoporosis. As the bones begin to lose minerals that provide structural support, the skeleton gradually becomes brittle and prone to fractures.
It is estimated that more than 200 million people worldwide are suffering from osteoporosis.
Bone fractures caused by osteoporosis have become very costly and dangerous, as this disorder is responsible for about 2 million fractures each year. Many people who have a fracture related to osteoporosis also spend considerable time in the hospital and in rehabilitation. This is particularly the case for adults over the age of 50 with osteoporosis, who may need to spend extended periods of time in a nursing home to receive proper care.
Furthermore, a person with a hip fracture has a 20 percent chance of dying within six months to one year following the fracture. The incidence of death after a hip fracture is higher in men than in women.
This guide will help you understand:
- what happens to your bones when you have osteoporosis
- how health care professionals diagnose the condition
- what you can do to slow or stop bone loss
- JointPro Physical Therapy’s approach to rehabilitation
Anatomy
What happens to bones with osteoporosis?
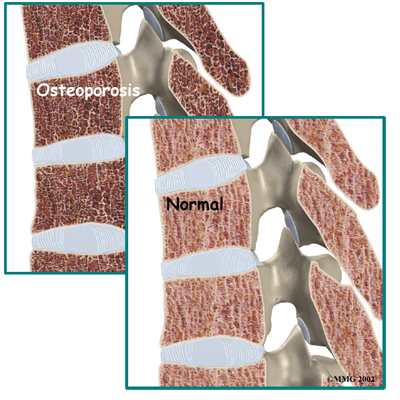
Most people think of their bones as completely solid structures that do not change. This is not true. The body is constantly replacing old, brittle bone tissue with newer, healthier bone tissue. In addition, your bones are constantly changing in response to the way you use your body. As muscles get stronger, the bones underneath them also get stronger. As muscles lose strength, the bones underneath them weaken. Changes in hormone levels or immune system function can also change the way the bones degenerate and rebuild themselves.
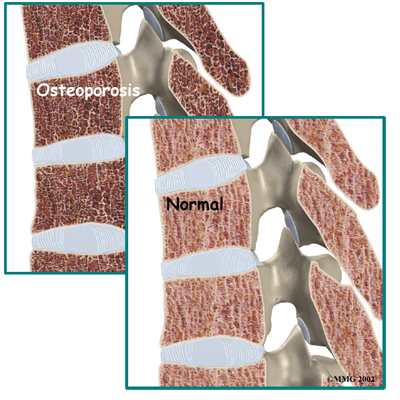
During childhood, your bones grow continuously and get denser (thicker). By about age 25, you hit your peak bone mass. As an adult, you can help maintain peak bone mass by staying active and eating a well-balanced diet that supplies ample amounts of calcium and vitamin D. Unfortunately, maintaining optimal bone mass gets harder as we get older. The natural aging process makes building strong bones more difficult due to changes in metabolism, hormone production, and dietary needs. In women, decreased estrogen production at menopause can also cause bones to lose density or mass very rapidly.
Throughout childhood, adolescence, and adulthood, bone cells called osteoblasts are responsible for building new bones. Stimulating the production of osteoblasts helps your body develop bone tissue, strengthen bones, and improve bone mineral density (the mineral content that supports bone structure). Old, brittle bone is broken down by bone cells called osteoclasts, and the activation of osteoblasts helps replace old bone. However, abnormal osteoclast activity can speed up bone loss.
In high-turnover osteoporosis, the osteoclasts reabsorb brittle bone tissue very quickly. This makes it difficult for osteoblasts to produce new bone fast enough to keep up with the osteoclast-related bone degeneration. The result is the significant loss of bone mass, particularly at the end of long bones (joints) as well as trabecular bone, which is the spongy bone inside vertebral (spinal) bones.
Postmenopausal women tend to have high-turnover osteoporosis (also known as primary type one osteoporosis). This is mainly due to the sudden decrease in estrogen production that occurs after menopause. Bones in the spine and wrist that are weakened by this form of osteoporosis are most prone to fractures.
In low-turnover osteoporosis, osteoclasts are working at their normal rate, but the osteoblasts still aren't forming enough new bone. Aging adults tend to have low-turnover osteoporosis (also known as primary type two osteoporosis). Hip fractures are most common in people with this type of osteoporosis.
Secondary osteoporosis refers to bone loss that is caused by, or secondary to, another medical problem such as a hormonal imbalance, certain bone cancers, and serious conditions that lead to inactivity. These types of health issues interfere with normal osteoblast function and cause over activity of osteoclasts. Some medications, especially corticosteroids that are used long-term, are known to cause secondary osteoporosis due to their impact on bone turnover.
Osteoporosis basically creates weak bones. When these weak bones are stressed or injured, they often fracture. Fractures most often occur in the hip or the bones of the spine (the vertebrae). They can also occur in the upper arm, wrist, knee, and ankle.
Causes
What causes osteoporosis?
Aging is one of the main risk factors for osteoporosis and osteoporotic fractures. If you are lucky enough to live a long and healthy life, you are much more likely to develop weakened bones from osteoporosis. In women, the loss of estrogen at menopause causes bone loss of up to two percent per year. White women over the age of 50 have a lifetime risk of fracture of about 50 percent. This percentage increases as women get older.
A number of factors contribute to or put you at risk of developing osteoporosis:
- advanced age
- female gender
- recent weight loss
- history of fractures
- family history of fractures
- tobacco use
- alcohol abuse
- lack of exercise
- low body weight or a thin and slender build
- extended use of certain medications (e.g., corticosteroids, anticonvulsants, and thyroid medicine)
- eating disorders such as anorexia or bulimia
- Asian or White race
These risk factors are just as relevant as a bone mass measurement in determining how likely you are to have a fracture. People with low bone mass who do not have additional risk factors do not typically develop fractures. However, individuals with minimal amounts of bone loss but several risk factors are more likely to suffer from fractures.
Symptoms
What does osteoporosis feel like?
Fractures caused by osteoporosis are often painful. Osteoporosis itself, however, has no symptoms. It is often called the ‘silent disease’ or ‘silent thief’, as many people don’t realize they have it until a fracture occurs. For this reason, it is especially important to get tested if you are a woman past menopause and have any common risk factors. Women over 65 should be tested regardless of whether they have risk factors. People with other bone problems or who take drugs that weaken the bones should also be tested. The initial screening for osteoporosis is painless and easy.
Diagnosis
How do health care professionals diagnose osteoporosis?
Free osteoporosis screenings that estimate your bone density measure (BDM) are available in many drug stores and malls. Most of these screenings use a machine that scans the bone in the heel of your foot. It is a fast and simple way to get an idea of your bone density. However, this test is not entirely accurate. Due to the heel bone bearing a lot of weight in normal activity, the test may show normal bone in the heel, even though the hipbones or spine may have low bone density. If however the foot scan shows a low bone mass, you should talk to your doctor. If the scan is negative however, and you suspect you may have osteoporosis or have some of the risk factors for developing the disease that are listed above, it is still recommended that you consult with your doctor.
When visiting your doctor he or she will take a detailed medical history to help weigh your risk factors for osteoporosis. If osteoporosis is suspected or you are at risk of developing it, your doctor may also recommend more precise testing. A bone density test, or in medical terms a dual-energy X-ray absorptiometry (DEXA) test is the most common method of measuring bone mass. A DEXA test is painless and uses special X-rays of the bones of your hip and spine to show your bone mass in these areas. The bone mass is then compared to that of a healthy thirty-year-old, called a T score. If you are within one standard deviation (SD) for bone density, you have normal bone. (SD is a statistic to measure variations in how a group is distributed.) If you are between one and 2.5 SDs below ideal levels, you are considered to be osteopenic. This means you have a mild form of osteoporosis. If the bone mass is more than 2.5 SDs below ideal levels, you have osteoporosis.
Unfortunately a single DEXA scan cannot show your doctor whether your bone mass is stable, increasing, or decreasing. Your doctor may have you take certain medications that create markers in the blood or urine to show what is happening in your bones. These tests will tell your doctor if you have high-turnover or low-turnover osteoporosis.
Be aware also that DEXA scans are not perfect. Different equipment or different technicians can get somewhat different readings. If you need to have more precise data, your doctor may recommend additional types of scans or tests.
Although a DEXA scan is the most common method of measuring bone density, other tests such as ultrasound, quantitative computed tomography (CT) scans, or single-photon absorptiometry may also be used instead of or in addition to the DEXA scan to confirm the diagnosis of osteoporosis.
If bone density tests show that you have weakened bones, your doctor will need to rule out other causes for this other than osteoporosis. In some cases, problems with bone marrow or hormone levels can cause bone loss. Blood tests can show these conditions.
In other cases the bone weakening is actually from a condition called osteomalacia.
Osteomalacia involves a softening of the bones caused by a lack of vitamin D. Vitamin D in your body comes from food and sunlight. Due to a lack of sunlight, almost 10 percent of people with hip fractures in the northern parts of the world have osteomalacia rather than osteoporosis. Urine and blood tests can help rule out osteomalacia.
In some cases, your primary care physician may refer you to a doctor who specializes in osteoporosis. For instance, if you are on medication to prevent bone reasbsorption and still have significant bone loss you may need to see a specialist. Referral is also advised for patients who have recurring fractures during therapy or repeated, unexplained fractures. Your doctor will help you find the right specialist for your situation.
Treatment Options
What can be done for osteoporosis?
The goal of your treatment plan will be to prevent fractures. This is especially important if you've already suffered from a fracture due to osteoporosis. To reduce the incidence of fractures, you need to increase your bone mass. If you have high-turnover osteoporosis, you also need to prevent rapid bone degeneration.
You need to take several steps to increase bone mass:
- If you smoke, quit immediately.
- If you drink alcohol, do so in moderation.
- Make sure you get enough calcium and vitamin D through the foods you eat. Adequate vitamin D intake helps your body absorb calcium and transport it to your bones.
- Eat enough calories to maintain a healthy weight. Being too thin increases your risk of osteoporotic fractures. Weight loss can be a cause of bone loss.
- Exercise regularly because your bones are constantly adjusting to the demands you put on them. Even low levels of exercise can help you maintain better bone mass. Low-impact exercises, muscle-strengthening exercises, and balance training are all recommended (see section below.)
Researchers believe that increased calcium intake alone, through a healthy diet, could reduce the number of fractures by 10 percent. Many people don't get enough calcium or vitamin D, especially as they get older. Sometimes it is difficult to get the recommended levels of essential nutrients from the food we eat, so supplements may become necessary, but remember to talk to your doctor about what kind of supplements to use.
Calcium comes in many forms. For example, calcium carbonate, calcium citrate, and calcium phosphate can be found in bone meal. The amount of calcium that is taken daily should be monitored by a doctor because if the body does not transport calcium properly, it can lead to a health issue known as calcification.
Calcification is a process in which calcium accumulates in the bloodstream as well as body tissue, where it can cause tissue to harden. Certain disorders may cause calcium to leak out of your bones or prevent the bones from absorbing calcium when it is taken in supplement form. If this happens, calcium starts to build up in areas where it doesn’t belong. Without proper treatment, various complications may develop due to calcification. This is why it is important to speak with your doctor when taking calcium supplements. Obtaining extra calcium and vitamin D through the foods you eat helps improve the effectiveness of all other treatments for osteoporosis, including physical therapy.
Physical therapy
Patients with osteoporosis or those at risk of developing this condition will benefit from working with a physical therapist at JointPro Physical Therapy.
The goals of our physical therapy treatment are to:
- Educate you about proper posture
- Teach you safe ways of moving and lifting
- Show you exercises you can do at home to help reduce the loss of bone mass and prevent fractures
The exercises we prescribe will particularly focus on activities that help increase the strength of your bones, as well as exercises that help maintain or improve your balance. Learning how to maintain optimum balance decreases your risk of falling, which can easily fracture an osteoporotic bone. We will also suggest exercises for your flexibility to help decrease stress that is typically placed on the bones by tight muscles. In addition, the therapeutic exercises we recommend can help improve your overall mobility.
If you have experienced a fracture due to osteoporosis, physical therapy at JointPro Physical Therapy can also help control your pain and allow you to gradually return to your regular activities. One of the most important aspects we aim to correct during therapy is poor posture.
Maintaining good posture is of utmost importance if you have osteoporosis. A curved upper spine posture, called kyphosis, is common in osteoporosis due to the wedge-like fracturing of the thoracic spine (middle portion of your spine) that often occurs. This type of injury develops when the front part of the vertebrae (spinal bones) collapse leaving the posterior portion (back of the vertebrae) in a higher position, creating a wedge-like appearance. These types of fractures cause the loss of height.
For this reason, accurately measuring and recording your body height is a key part of our physical therapy evaluation. A height measurement gives your physical therapist an idea of how osteoporosis is affecting your bones and posture, and comparing the recordings over a period of time can help us track your success with treatments.
With posture exercises, the goal is to get your body lined up from head to toe, with weight going through your hips. In a healthy spine posture, the head is balanced on top of the spine, rather than tilted forward, which is common in osteoporosis.
In people with advanced osteoporosis, the upper body is also commonly bent forward at the hips. This prevents the hip bones from maintaining proper trunk positioning, which causes too much weight and stress to be placed on the hips. As a result, the bones weaken and become more prone to fracture. It is therefore important at all times to try to “stand tall,” as this can both prevent the loss of height and help you regain height lost from a fractured osteoporotic spine.
Your physical therapist will describe different strategies that can help you put good posture into practice. This is called body mechanics, which is the way you align your body while performing daily activities. Remember that a healthy posture is balanced with the body aligned from the head to toe. The same posture should be used when you bend forward to pick up objects. Instead of rounding out your shoulders and upper back, keep the back in its healthy alignment as you bend forward at the hip joint. This keeps your back in a safe position.
When bones are weakened from osteoporosis, rounding the spine forward while bending and lifting pinches the front section of the vertebrae and increases the risk of a spine fracture. This pinching is exacerbated when any weight is lifted in this position. Even the weight of a purse or shopping bag can add detrimental stress to an osteoporotic spine, leading to a fracture. Along with maintaining proper posture, gently tightening the muscles around your core area can also help protect the back during activities such as lifting. Your physical therapist will educate you on how to use your core muscles to protect your spine. Individuals with an osteoporotic spine who rapidly bend forward, such as that experienced when one sneezes or coughs, can be enough to cause a spinal fracture. Due to this issue, your physical therapist will educate you on consciously extending your back instead of flexing your spine during these activities.
Another motion that is particularly stressful for an osteoporotic spine is a twisting motion. The normal structure of bone is not designed to withstand twisting very well, and combined with the weakened bone state of osteoporosis the twisting motion can easily cause a fracture. Although it is difficult to eliminate twisting movements from everyday life, this movement should be avoided whenever possible, especially for activity that requires higher-velocity motions such as a golf swing, tennis swing, or bowling action. In addition to learning posture exercises that can be used for everyday movements, strengthening exercises for your bones are also an important part of maintaining the health of osteoporotic bones.
Remember that as your muscles get stronger, the bones underneath them also get stronger as they react to the added stress placed on them. In this way, strength training and weight-bearing activities force the bones to build mass. Your physical therapist will prescribe some gentle weighted exercises, using either elastics or weights, for your upper and lower extremities. Using an appropriate weight is vital and your physical therapist can educate you on how much resistance is appropriate for you.
If you are using free weights, handling the weights is just as important as doing the actual exercises. Never lift weights in the flexed forward posture that was described above, and be careful to gradually increase the resistance you use, as weights that are too heavy will gradually cause your body to slip into the flexed forward posture that is detrimental to people with osteoporosis. Performing exercises while your upper back is properly supported by good postural alignment is also recommended to avoid added stress on the thoracic spine.
Exercises that involve flexing the spine, such as toe touches, abdominal crunches, and dead lifts, should strictly be avoided. Carefully guided strengthening exercises for your upper back will be encouraged by your physical therapist to counteract curved forward posturing.
Weight-bearing cardiovascular exercises such as walking outdoors or on a treadmill, gentle non-pounding forms of dance, and stair climbing are useful activities that help balance weight placed on the bones. These exercises also encourage an upright posture while improving cardiovascular health.
Although a lot of people enjoy cycling, it is not a recommended activity as it does not provide the benefits of weight bearing and it also causes the detrimental flexed forward posturing of the spine. In addition, pool exercises are not weight bearing, so they are not recommended unless severe pain from osteoporosis limits physical activity on the ground, in which case exercising in the pool would be acceptable and recommended. High-impact activities such as running, jumping, and stomping forms of dance should be strictly avoided. Your physical therapist at JointPro Physical Therapy can educate you on safe cardiovascular activities specific to your interests and physical needs.
The next part of our treatment will focus on your balance. Poor balance can lead to a fall, which can easily fracture an osteoporotic bone. In some cases, a fracture from a fall can be a potentially life-threatening situation. Exercises that help improve your balance can be as simple as standing with your feet close together, standing on one foot, or standing with one foot in front of the other. Closing your eyes can make any of these activities even more challenging, but in a beneficial way. By challenging your body, your reaction time to unexpected situations such as tripping will improve and your likelihood of falling will decrease. The most important aspect of improving your balance is ensuring that you are doing it in a safe environment. Your physical therapist will provide you with exercises that are specific to your current level of balance. As your balance gets better, more challenging exercises will be provided. Tai chi, which is an exercise form originating in China, is a great way to enhance balance, and many patients benefit from practicing this activity on a regular basis.
The final component of our treatment at JointPro Physical Therapy is to provide you with flexibility exercises. By improving and maintaining your flexibility, the stress put on your bones by tight muscles will decrease and the ability to practice good posture and body mechanics will increase. Heightened flexibility also improves your mobility, which in turn enhances your balance and decreases your risk of falls. In addition, stretches for your upper back and chest will be prescribed to decrease the likelihood of developing a curved posture. Stretches for your hips, calves, and neck are also important if you have osteoporosis and will be included in your stretching regimen.
Your physical therapist will continue to compare your test results for body height, posture, strength, balance, and flexibility to see how well you are progressing and to encourage you to continue with your exercise program. Once you can safely and proficiently perform your home exercise program, regular visits to JointPro Physical Therapy will not be required. However, we will continue to be a resource for any further questions you may have or problems you may encounter.
If you are seeing one of our physical therapists at JointPro Physical Therapy because you have recently had a fracture related to osteoporosis, our treatment will initially focus on decreasing your pain. We may use hands-on treatment as well as modalities such as ice, heat, ultrasound, or electrical current to assist in managing your pain. We will liaise with your doctor to determine the best time to begin more advanced exercises involving strengthening, balance, and flexibility, and will proceed with them when appropriate to allow you to return to your normal activities as quickly as possible.
JointPro Physical Therapy provides services for physical therapy in Frankfort, New Lenox.
Medication
Depending on your situation, your doctor may prescribe medications to slow down your body's degeneration of bone.
Many medications are now available for the prevention and/or treatment of osteoporosis. When a doctor is trying to determine the appropriate medication for each patient, the benefits and risks of the medication are taken into consideration. These are weighed against specific patient characteristics and risk factors. Ultimately, the best medication is the one most likely to be taken consistently and correctly by the patient.
If you are past menopause, hormone replacement therapy may be effective. Bisphosphonates and calcitonin can also slow your body's degeneration of bone. Studies have shown that 80 percent of women actually build bone mass up to two percent per year while on estrogen replacement therapy. Estrogen replacement has also been shown to decrease the occurrence of fractures in the vertebrae by 50 percent and fractures in the hip by 25 percent. Fortunately, studies have also shown that hormone replacement therapy can help lower the rates of coronary artery disease (heart disease), relieve some symptoms of menopause, and maybe even prevent or postpone Alzheimer's disease.
Hormone replacement therapy often worries many women because studies have shown that it may increase the risk of breast cancer. For women with a family history of breast cancer or those who have had a stroke or thrombophlebitis (blood clots), hormone replacement therapy is not recommended. However, women who are candidates for this treatment should consider taking estrogen because its positive effect on osteoporosis is significant. Researchers estimate that if estrogen were widely used, it could reduce all osteoporotic fractures by 50 to 75 percent.
It is important to note that hormone replacement therapy must be continued to be effective. When a woman stops taking estrogen, she'll start to lose bone at a very fast rate again. Within seven years, her bone density will be as low as that of a woman who has never taken estrogen.
Another form of intervention for women who are at least five years postmenopausal is calcitonin treatment. Doctors often prescribe calcitonin to patients with fractures. Calcitonin is a non-sex, non-steroid hormone. This hormone binds to osteoclasts (the bone cells that degrade and reabsorb bone), to decrease their numbers and activity level. Calcitonin used to be administered only by injection, but now it is available in a nasal spray and a rectal suppository. Nasal calcitonin is most often used for women with osteoporosis who are five years or more past menopause and unable to take other approved agents. For reasons that are not clearly understood, calcitonin also seems to relieve pain.
You and your doctor need to work together to monitor the effects of calcitonin. It is a newer form of treatment, and its long-term effects as well as benefits are not fully known. In addition, more than 20 percent of patients develop a resistance to calcitonin over time, and it stops working for them.
Bisphosphonates also slow bone degeneration and reabsorption by blocking osteoclasts. Some common bisphosphonates are Alendronate (Fosamax), Risedronate (Actonel), or Ibandronate (Boniva).
Bisphosphonates may be taken orally (in pill form) on a daily basis. Others are available in weekly or monthly doses. A new injectable bisphosphonate (Zoledronate) can be given annually (once a year). Boniva comes in pill form and can also be injected once every three months. The injectable forms of these medications are used in the management of postmenopausal osteoporosis.
Studies have shown that bisphosphonates increase bone mass and prevent fractures. Furthermore, discontinuing the medication doesn't seem to cause the rapid bone loss that occurs when a patient stops taking estrogen. However, it is not clear how well bisphosphonates work when used for a long time. Due to the potential side effects of these medications, you need to liaise closely with your doctor if you take them.
Another drug that may be used to treat osteoporosis is Raloxifene (Evista), which is an anti-estrogen. Anti-estrogens are also called selective estrogen-receptor modifiers (SERMs). This form of drug improves bone density and prevents fractures in a similar manner as estrogen, but without increasing the chances of hormone-related cancers. The main benefit of SERMs over hormone replacement therapy is that they do not increase the risk of breast cancer.
Raloxifene is frequently used for postmenopausal women under the age of 65. They must not be at risk for blood clots or have cardiovascular disease. Furthermore, men may be prescribed the only anabolic agent (Teriparatide/Forteo) approved for the management of osteoporosis. Anabolic usually refers to hormones that build up muscle or bone mass. Forteo is a form of parathyroid hormone used for patients who have a high risk of fracture. The use of an agent with antiresorptive effects, such as a bisphosphonate, usually follows Forteo treatment.
New drugs that may be beneficial for the treatment of osteoporosis are currently being researched. Some of these drugs, such as sodium fluoride, can be helpful in low-turnover osteoporosis. These drugs reinforce osteoblast activity by helping them create more bone. Sodium fluoride may be available for treatment purposes in the near future.
Lifestyle changes, hormone replacement therapy, prescription medications, regular exercise guided by a physical therapist, and recent advances in drug therapy can help you take control of your osteoporosis. You and your doctor should be able to find ways to help you prevent the debilitating fractures of osteoporosis.
Portions of this document copyright MMG, LLC.